Gastric Reflux Surgery
What is Heartburn or Gastric Reflux?
Gastro-oesophageal reflux is a condition that develops when the reflux of stomach contents causes troublesome symptoms and/or complications. It is manifested by a spectrum of nonspecific symptoms, including heartburn, regurgitation, dysphagia, laryngitis, dental problems, adult-onset asthma, and/or aspiration pneumonia.
Some degree of reflux is physiologic. Physiologic reflux episodes typically occur postprandially, are short-lived, asymptomatic, and rarely occur during sleep.
Pathologic reflux is associated with symptoms of mucosal injury and often occurs nocturnally.
Normally, the stomach contents are retained with the help of the lower oesophageal sphincter (LOS), a muscle that contracts and relaxes to maintain the one-way movement of food. However, gastro-oesophageal reflux disease develops when anti-reflux mechanisms that are normally in place are disrupted.
Causes of Gastric Reflux
Several factors contribute to the development of pathologic reflux, including:
- Obesity
- Hiatus Hernia
- Smoking
- Pregnancy
Common foods such as alcohol, spicy foods, onions, chocolates, caffeine-containing drinks, mints, tomato-based foods, citrus fruits and certain medications can worsen gastric reflux.
Impact of Gastric Reflux
Living with gastric reflux is inconvenient as symptoms can severely interfere with your life. You may have to follow certain dietary restrictions, and reflux occurring in the night can hinder a good night's sleep, thereby affecting alertness and productivity the next day.
Long-term complications can include:
- Erosive oesophagitis
- Barrett’s oesophagus
- Oesophageal stricture
- Asthma
- Chronic laryngitis
- Laryngeal and tracheal stenosis
- Chronic cough
- Dental erosions
- Chronic sinusitis
- Recurrent pneumonitis
- Increased risk of oesophageal adenocarcinoma
Symptoms of Gastric Reflux
Heartburn is usually the main symptom of GORD, characterised by a burning-type pain in the lower part of the mid-chest, behind the breastbone.
Other symptoms include:
- a bitter or sour taste in the mouth
- trouble swallowing
- nausea
- dry cough or wheezing
- regurgitation of food
- hoarseness or change in voice
- chest pain
Diagnosis for Gastric Reflux
Your doctor may order some of the following tests to diagnose gastric reflux:
- Endoscopy: Allows the doctor to examine the inside of your oesophagus, stomach and portions of the intestine with an instrument called an endoscope, a thin, flexible telescope.
- pH testing: Involves inserting a tube through your nose into the oesophagus and positioning it above the LOS. The tube tip contains a sensor that can measure the pH of the acid content refluxed into the oesophagus. The tube will be left in place for 24 hours.
- Oesophageal Manometry: A tube placed into the oesophagus measures how well the muscles of the oesophagus work, which helps assess the problem.
- Barium oesophageal
- Gastric emptying study
Treatments for Gastric Reflux
Treatment aims to reduce reflux, relieve symptoms and prevent damage to the oesophagus. Some of the treatment options include:
- Lifestyle modification: this includes weight loss, the elevation of the head of the bed, elimination of dietary triggers, avoiding lying down within 90 minutes of eating, and avoiding alcohol and tobacco. : Medications: either over-the-counter or prescription medication with antacid effects
- Antireflux surgery: Surgical management of GORD focuses on restoring a physiologic equivalent to the normal lower oesophageal sphincter. Manometric studies correlate GORD with a lower mean LOS pressure, shorter mean intra-abdominal LOS length, and shorter overall sphincter length. Specific surgical procedures can correct each of these problems.
What is Gastric Reflux Surgery?
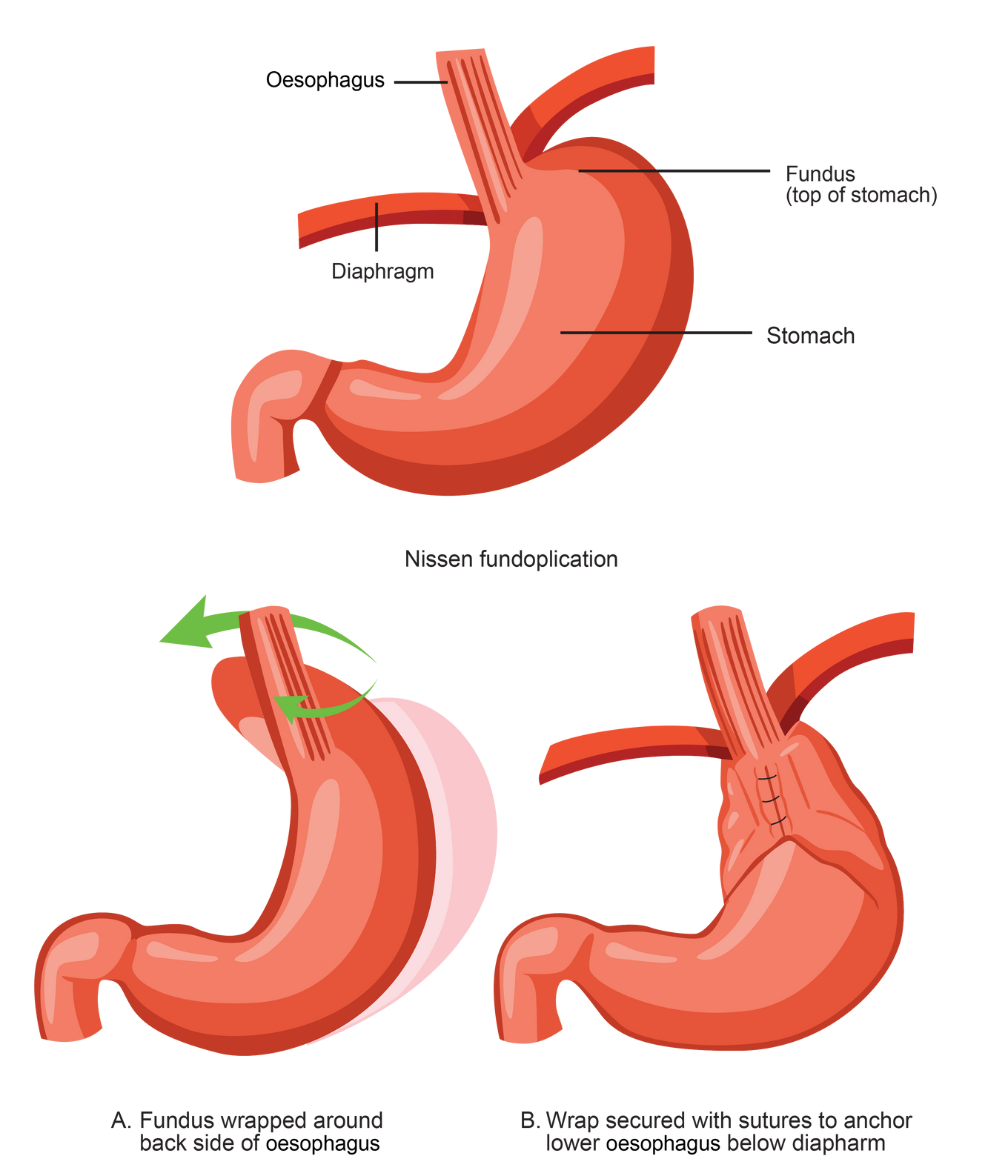
Gastric reflux surgery, also known as anti-reflux surgery, is a surgical procedure to treat gastroesophageal reflux disease (GORD). Gastric reflux surgery generally includes fundoplication, a technique to recreate lower esophageal sphincter pressure by wrapping the fundus of the stomach around the oesophagus in the abdomen.
It involves repairing the malfunctioning lower esophageal sphincter (LES), which prevents the backward flow of stomach acid into the oesophagus. By restoring the normal function of the LES, gastric reflux surgery aims to alleviate the symptoms and complications associated with GERD.
Fundoplication Surgery for GORD
If conservative treatment options fail to resolve your GORD, your doctor may recommend a surgical procedure called Fundoplication. Fundoplication surgery reinforces the lower oesophageal sphincter’s ability to close and helps to prevent gastro-oesophageal reflux from occurring. This surgery can be performed laparoscopically through tiny incisions in the abdomen in most people.
Benefits of Fundoplication Laparoscopy
Laparoscopy is much less traumatic to the muscles and soft tissues than surgically opening the abdomen with long incisions. It is also associated with a shorter hospital stay, less postoperative pain and faster recovery.
Who is Suitable for Gastric Reflux Surgery?
Antireflux surgery is typically recommended for individuals who experience chronic GORD symptoms unresponsive to conservative treatments, such as lifestyle modifications and medication. Suitable candidates for gastric reflux surgery may include those with severe symptoms, complications of GERD (such as Barrett's oesophagus), volume reflux or individuals who wish to reduce their reliance on long-term medication. It is also indicated for patients with non-gastrointestinal symptoms such as chronic cough, laryngeal disease and asthma when there is solid objective evidence to attribute such symptoms to reflux.
Benefits of Gastric Reflux Surgery
Gastric reflux surgery offers several benefits for individuals with chronic GERD, including:
- Relief from GORD Symptoms: Alleviate symptoms such as heartburn, regurgitation, chest pain, and difficulty swallowing, providing significant relief and improving quality of life.
- Reduced Medication Dependence: For individuals who rely on long-term medication to manage GERD, surgery may reduce or eliminate the need for daily medication, offering a more sustainable solution.
- Improved Oesophageal Health: By preventing the backward flow of stomach acid into the oesophagus, gastric reflux surgery can help prevent complications such as esophageal inflammation, ulcers, and the development of Barrett's oesophagus.
What to Expect After Gastric Reflux Surgery?
After gastric reflux surgery, patients can expect the following:
- Hospital Stay: Most patients can expect to stay in the hospital for a day or two after the surgery to monitor their recovery and manage postoperative discomfort.
- Diet Progression: You will start with a liquid or soft diet and gradually transition to solid foods as guided by your surgeon or dietitian.
- Recovery and Healing: It may take several weeks for the incisions to heal completely, and you should follow your surgeon's instructions regarding activity restrictions and wound care.
Gastric Reflux Surgery Care Plan
Wound Care
- You will be given instructions as to how to care for your incisions.
Pain Management
- You may feel soreness around the incision areas. As (during the procedure), the abdomen was distended with gas.
- Your surgeon may prescribe pain medicine or recommend paracetamol for the first few days to keep you comfortable.
- You may experience discomfort in the abdomen, chest, or shoulder area for several days.
Activity
- Shortly after surgery, you can gradually resume your daily activities.
- You are encouraged to start walking as early as possible to reduce the risks of blood clots and pneumonia.
- You are advised not to lift heavy objects for four weeks.
Work
- You can get back to work in 7-10 days.
Gastric Reflux Surgery Prognosis
The outcome of treatment varies from person to person. Surgery is beneficial in approximately 90% of patients. Many patients who have suffered for years from heartburn and required medication to control the symptoms find that all symptoms are alleviated as soon as they awake from surgery and no longer need medication. Some may experience mild symptoms.
While treatment can be very successful for others, most people respond well to lifestyle changes and medications. However, relapse is very common after cessation of medications, so the condition does require maintenance. Surgery is recommended when medications fail to resolve symptoms or you prefer not to take them.
Gastric Reflux Surgery Risks
As with any surgical procedure, gastric reflux surgery carries potential risks and complications, including infection, bleeding, adverse reactions to anaesthesia, damage to surrounding structures, and post-operative discomfort. Fundoplication may involve certain side effects. These can include trouble swallowing, inability to burp or vomit, bloating and passing more wind. Most patients experience some weight loss after the procedure.








