Mini Bypass
What is Mini Gastric Bypass?
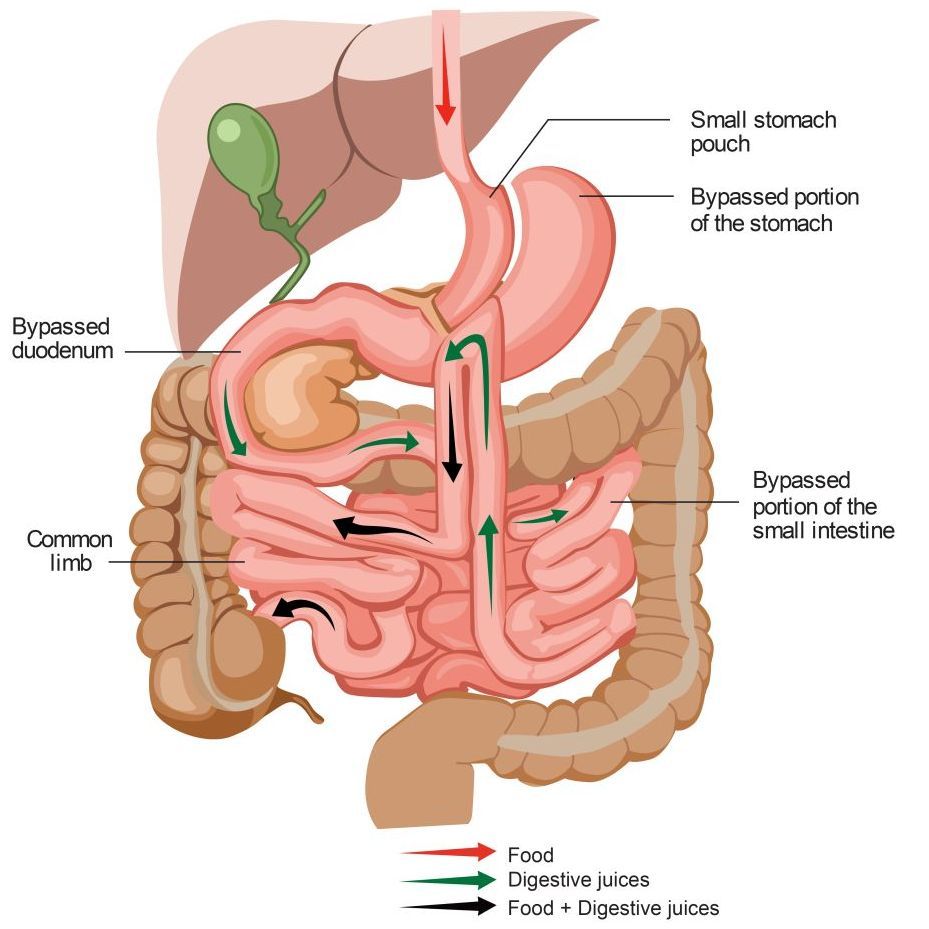
A mini gastric bypass procedure, also known as a one anastomosis gastric bypass, is a surgical procedure that involves the creation of a long, narrow gastric pouch that is then connected (anastomosed) to the small intestine, bypassing approximately 150 cm of the upper part of the small intestine.
Who is Suitable for a Mini Gastric Bypass?
You may be eligible for a gastric bypass if you:
- Meet criteria for weight loss surgery (see ‘Am I a candidate?’)
- Have significant gastroesophageal reflux
- Require a revision procedure after bariatric surgery, such as gastric banding or sleeve gastrectomy.
Benefits of mini gastric bypass
The benefits of mini gastric bypass approach include:
- It is particularly effective for patients with a larger BMI and has better weight loss outcomes than Roux-en-Y.
- It is a simpler operation than Roux-en-Y and has favourable perioperative morbidity.
- Most patients have an almost immediate reduction in their need for diabetic medication, and some can completely stop diabetic medication altogether.
- It does not require any ongoing adjustments, which are required with other procedures, such as the gastric band. Regular follow-up is, however, necessary to ensure weight loss is appropriate and intake is nutritionally adequate.
- It is effective for those people who tend towards high-sugar or high-fat foods. Dumping syndrome is directly linked to a high-sugar or high-fat intake.
- This procedure does not require resection of the bowel or stomach
Alternative Options
While the mini gastric bypass is an effective weight loss intervention, it may not suit everyone. Alternative options for weight loss include:
- Gastric Sleeve Surgery: This involves removing a portion of the stomach to create a smaller, banana-shaped stomach pouch, promoting weight loss.
- Roux-en-Y gastric bypass
- SADI
- Adjustable Gastric Banding: This involves placing a silicone band around the upper part of the stomach to create a smaller pouch, limiting food intake. The band can be adjusted over time to achieve the desired level of restriction.
- Medical Weight Management Programs: These programs provide comprehensive support and guidance for weight loss through dietary counselling, exercise plans, behaviour modification strategies, pharmacotherapy and ongoing monitoring by healthcare professionals.
- Lifestyle Modifications: Healthy lifestyle habits, such as a balanced diet, regular exercise, and behaviour changes, can contribute to weight loss and improved overall health.
The Procedure
- The procedure is performed with a laparoscopic (keyhole) technique under general anaesthesia.
Five small incisions (between 5 and 12mm long) are made to insert keyhole surgery instruments. - Using these instruments, the top of the stomach is stapled to form a thin tube (30ml to 50ml in size). The thin tube becomes the new, smaller stomach completely separate from the rest.
- This stomach is then sewn to a loop of the small intestine, bypassing the first part of the intestine called the duodenum and approximately 150 of the small bowel. The remnant stomach and upper part of the small intestine remain in the body but are no longer used for food digestion.
What to Expect After Surgery
The postoperative period is crucial for a successful recovery and long-term weight loss. Here are some common aspects of the post-operative phase following MGBP:
- Hospital Stay: Depending on your surgeon's recommendation and your circumstances, you may be required to stay in the hospital for up to three to five days after the surgery. This allows medical professionals to monitor your progress and ensure a smooth recovery.
- Pain Management: Your healthcare team will provide appropriate pain management strategies, including medications and other techniques, to help alleviate discomfort and promote comfort.
- Dietary Progression: Your diet will progress gradually from clear liquids to pureed foods and eventually solid foods as guided by your healthcare team. This allows the digestive system to heal and adapt to its new structures.
- Lifestyle Changes: Healthy lifestyle habits, including regular physical activity and mindful eating, are crucial for long-term weight loss. Your healthcare team will guide you on incorporating these changes into your daily routine.
Post-Operative Care Plan
After the procedure, you will start on clear fluids only (water, black tea, broth, juices). These will need to be sipped slowly in small amounts. An x-ray study is performed after the operation to check the size of the stomach pouch and to exclude a leak from the new connection.
You will then be able to have free fluids for the rest of your hospital stay. During the next four to six weeks, while your body heals, you will gradually increase the texture and volume of the food you take. Further information, including a dietary guidelines booklet, will be provided at your appointment with the dietician.
Surgeon
The first postoperative clinic visit will be arranged for one to three weeks after surgery. Your wounds will be assessed at this appointment, and any other issues will be discussed.
Dietitian
Remember that surgery is an aid to weight loss. Eating behaviours must be modified to get the best result from the procedure. Eat various healthy foods, limit your calorie-dense foods and liquids, and slow your eating speed to improve food tolerance.
If eating behaviours are not adapted after surgery, weight loss will be limited, or weight regain can be possible. More detailed information about correct eating behaviours will be covered during your visit with the dietitian.
Risks
Complications of bariatric surgery may include general and specific complications. More common complications are listed below.
General complications:
- Anaesthetic complications
- Death
- Bleeding
- Pneumonia
- Wound infection
- Myocardial infarct
- DVT/PE (blood clots)
- Allergy
- Urinary infection
- Nausea and vomiting
- Other hospital-acquired infections, e.g. diarrhoea
- Injury to bowel or organs
- Incisional hernia
- Inadequate weight loss/weight regain
- Need for further surgery
- Malnutrition
- Oral intolerance
- Gallstones
- Conversion to open
Specific complications after a mini gastric bypass may include:
- Marginal ulcers
- Bile reflux
- Gastro-gastric fistula
- Stenosis of the anastomoses
- Bowel obstruction
- Internal hernia (rare)
- Anastomotic leak
- Bleeding from staple line or anastomosis
- Dumping
- Diarrhoea
- Chronic abdominal pain
- Bacterial overgrowth
- Hypoglycaemia