Single Anastomosis Duodeno–Ileal Bypass with Sleeve Gastrectomy (SADI-S)
What is SADI-S?
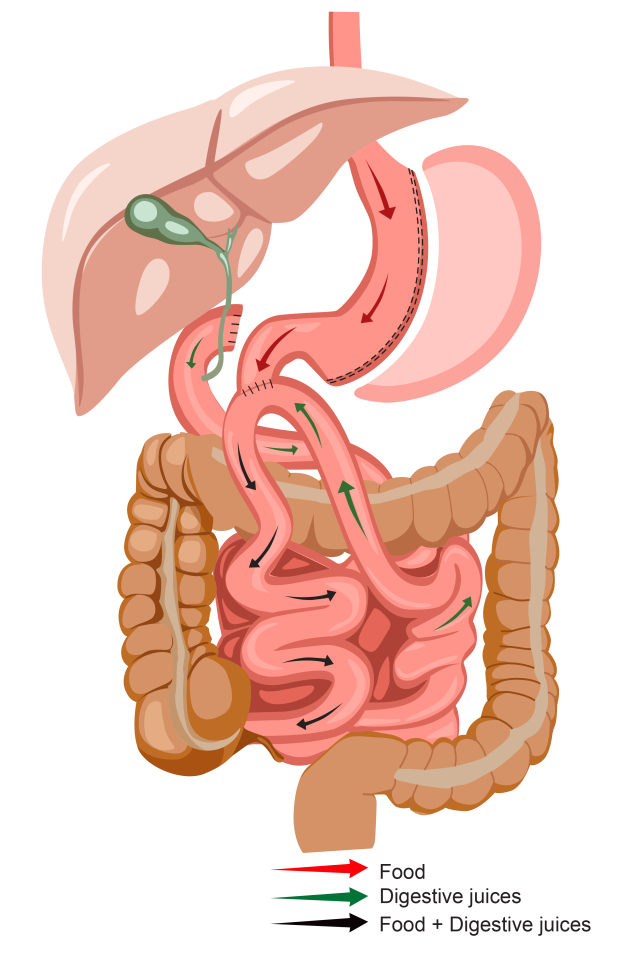
SADI-S (Single Anastomosis Duodeno–Ileal Bypass with Sleeve Gastrectomy) is a modified version of the duodenal switch. This procedure has been used to treat morbid obesity for over 30 years. SADI-S combines the benefits of sleeve gastrectomy and intestinal bypass. The loop configuration offers the opportunity to minimise the risk of marginal ulcers and internal hernia while simplifying the operation.
Sleeve gastrectomy removes 75% of the stomach resulting in a reduced capacity to eat and a reduced level of ghrelin, the hormone which causes hunger. Intestinal bypass involves dividing the top part of the small bowel (duodenum) just beyond the outlet of the stomach (pylorus) and joining the lower part of the small bowel (ileum) to this top part.
This results in food bypassing part of the small intestine, which causes a reduction in the absorption of nutrients consumed.
Who is Suitable for a SADI-S Surgery?
You may be eligible for a SADI-S if you
- Meet criteria for weight loss surgery (see ‘Am I a candidate?’)
- Have gastroesophageal reflux
- Have a higher BMI
- Have obesity-related metabolic comorbidities such as type 2 diabetes mellitus
- As part of a planned two-stage operation after sleeve gastrectomy
- Require a revision procedure after bariatric surgery, such as gastric banding or sleeve gastrectomy
- Demonstrate commitment to strict lifelong adherence to nutritional supplementation due to the higher rate of nutrient deficiencies
Advantages of SADI-S Surgery
Studies show SADI-S can provide greater weight loss than a standard sleeve gastrectomy or Roux-en-Y gastric bypass. Some other advantages of SADI-S include:
- Combines benefits of sleeve and bypass
- Excellent weight loss outcomes
- Less risk of dumping syndrome
- Less risk of internal hernia
- Less risk of marginal ulcers
- Minimal risk of bile reflux gastritis
- May improve reflux symptoms
- High rates of resolution of obesity-related comorbidities
- Lower rates of anastomotic complications compared to duodenal switch or Roux-en-Y gastric bypass
Alternatives to SADI-S Surgery
- Gastric Sleeve Surgery: This involves removing a portion of the stomach to create a smaller, banana-shaped stomach
- Roux-en-Y gastric bypass: This involves making a small gastric pouch and diverting food past the majority of the stomach and a small portion of the small intestine.
- Mini gastric bypass: This involves the creation of a long, narrow gastric pouch which is then connected (anastomosed) to the small intestine bypassing approximately 150 cm of the upper part of the small intestine.
- Adjustable Gastric Banding: This involves placing a silicone band around the upper part of the stomach to create a smaller pouch, limiting food intake. The band can be adjusted over time to achieve the desired level of restriction.
- Medical Weight Management Programs: These programs provide comprehensive support and guidance for weight loss through dietary counselling, exercise plans, behaviour modification strategies, pharmacotherapy and ongoing monitoring by healthcare professionals.
- Lifestyle Modifications: Healthy lifestyle habits, such as a balanced diet, regular exercise, and behaviour changes, can contribute to weight loss and improved overall health.
SADI-S Procedure
SADI consists of two steps. In the first one, called “sleeve gastrectomy”, the stomach is reduced and narrowed into a tube to reduce the stomach capacity.
In the second step, a small bowel bypass is performed to reduce the surface area available for food absorption. Specifically, the middle part of the small bowel is excluded from food transit. The first portion of the small bowel, the duodenum, is divided, and a loop of the small bowel (the portion known as the ileum) is connected (anastomosed) to the duodenum (on the stomach side). Thus, after this second step, the first part of the small bowel (the duodenum) is connected to the distal small bowel (the ileum).
In short, after this operation, food travels from the new narrow stomach to the distal intestine bypassing a long segment of the small bowel, which remains in the abdominal cavity but is excluded from food absorption. These anatomical changes decrease oral intake and reduce the absorption of the nutrients and calories eaten.
Postoperative Care Plan
Following your surgery, you will typically spend one night in the hospital and be administered pain-controlling medications to keep you comfortable.
You will be kept on a liquid diet for the first two weeks following your surgery. Drinking plenty of fluids throughout the day is important to avoid dehydration.
Your surgeon and dietician will give you a specific diet plan and instructions to follow after this.
After your first procedure, your diet will be strictly limited to clear liquids initially, then other types of liquids, such as protein shakes and non-fat milk, thereafter. You will follow our bariatric diet through its four stages (see ‘Healthy Eating’ after surgery. It is particularly important that you consistently take your multivitamins and any prescribed additional supplements after this procedure. Your nutrient levels will be closely monitored throughout your follow-up.
SADI-S Surgery Risks
Complications of bariatric surgery may include general and specific complications. More common complications are listed below.
General complications:
- Anaesthetic complications
- Death
- Bleeding
- Pneumonia
- Wound infection
- Myocardial infarct
- DVT/PE (blood clots)
- Allergy
- Urinary infection
- Nausea and vomiting
- Other hospital-acquired infections, e.g. diarrhoea
- Injury to bowel or organs
- Incisional hernia
- Inadequate weight loss/weight regain
- Need for further surgery
- Malnutrition
- Oral intolerance
- Gallstones
- Conversion to open
Specific complications after SADI-S may include:
- Marginal ulcer
- Anastomotic leak
- Staple line bleeding or leak
- Severe malnutrition
- Reflux
- Internal hernia (rare)
- Dumping (rare)
- Diarrhoea
- Need for reversal or additional operations
- Chronic abdominal pain
- Bacterial overgrowth
- Hypoglycaemia
- Long-term (>10 years) data not yet available








